What Is Testicular Cancer?
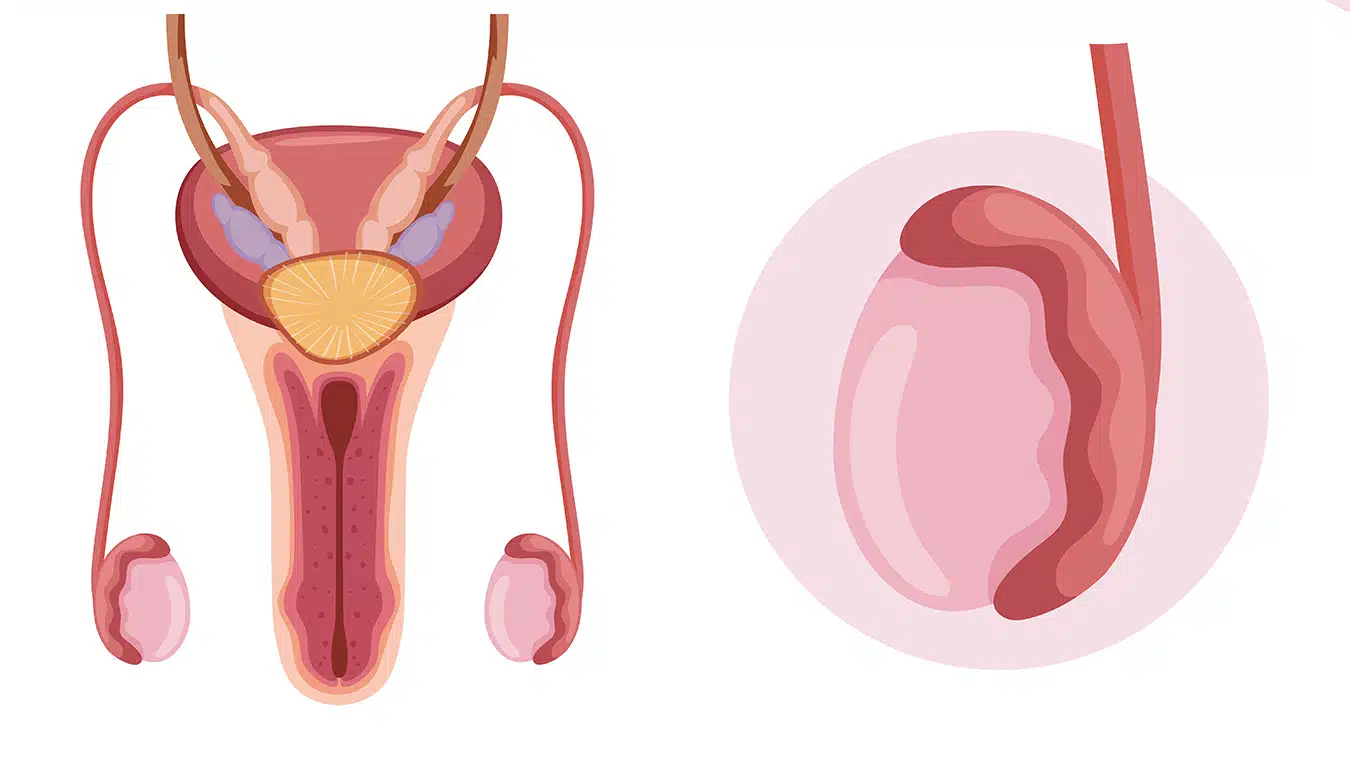
Testicles are a pair of egg-shaped organs located just below the penis and covered by the skin called the scrotum. The primary function of these organs is to produce sperm and testosterone. Testicular cancer is a type of cancer that occurs in the testicles. It is most commonly seen in adult males and is generally considered a relatively rare form of cancer.
Among the functions of the testicles are the production of semen for reproduction and the secretion of the male hormone, testosterone. While testicular cancer is relatively rare, it is known to be one of the most common organ cancers in males under the age of 35.
A family history of testicular cancer is highly significant if a man has this condition. If there is a history of cancer in a father or brother, it's important to be more vigilant and undergo the necessary tests regularly without neglect.
Most cases of testicular cancer can be treated with surgery and chemotherapy, and the overall survival rates are generally very high. Testicular cancers typically originate from cells called "germ cells," which are involved in sperm production. Testicles, which are located inside the scrotum and come in pairs, one on the right and one on the left, also produce the male hormone testosterone and play a vital role in the male reproductive system. In this article, we will share detailed information about testicular cancer.
What Are the Symptoms of Testicular Cancer?
Testicular cancer presents with various symptoms, with the most common being the painless presence of a lump in the testicles. Most testicular cancers do not cause pain, but some patients may experience discomfort. If there is any hardness or lump in the testicle, it is recommended to consult a specialist as soon as possible. Other symptoms of testicular cancer include:
- Enlargement and pain in the breasts
- Back pain
- Neck pain or lump
- Unexplained weight loss and fatigue
The exact cause of testicular cancer is not known, but there are some factors associated with an increased risk of developing it.
Risk factors include:
Cryptorchidism (Undescended Testicles)
Cryptorchidism, a congenital structural abnormality, increases the risk of developing testicular cancer by 4 to 8 times.
History of Testicular Cancer
Individuals who have previously had testicular cancer are at a significantly higher risk of developing a second testicular cancer.
Genetic Factors
Certain genetic conditions like Klinefelter syndrome, Down syndrome, and androgen insensitivity syndrome can increase the risk of testicular cancer.
Age
Most cancers, including testicular cancer, are more commonly diagnosed in men after puberty and in those under the age of 40. Additionally, men between the ages of 50 and 60 are also at risk.
Family History
Individuals with a first-degree relative (father or brother) who has had testicular cancer have a higher likelihood of developing the condition.
Early Diagnosis
There are no specific screening methods for testicular cancer. Typically, it is crucial for individuals to perform self-examinations regularly and seek medical attention if they detect any lumps in their testicles.
Generally, painless swelling and lumps in one or both testicles are the most common initial symptoms. It's important to note that various factors can cause the symptoms associated with cancer.
When testicular cancer metastasizes (spreads), different symptoms may occur. Lymph nodes, lungs, and the liver are some common sites of metastasis. When cancer cells spread to the lymph nodes, pain in the lower back region is commonly felt. Lung metastases may cause symptoms such as coughing, coughing up blood, shortness of breath, and chest pain. The most common symptom of liver metastasis is abdominal pain. In rare cases, testicular cancer can also metastasize to the brain, leading to severe headaches.
What Are the Diagnostic Methods for Testicular Cancer?
Several methods are available to confirm the diagnosis of testicular cancer in cases where a testicular mass is suspected. These methods include:
Scrotal Ultrasound
Scrotal ultrasound is an imaging technique used to determine whether a detected mass originates from the testicle itself or the surrounding tissues.
Blood Tests
Elevated levels of tumor markers specific to testicular cancer, such as Alpha-fetoprotein (AFP), Beta-human chorionic gonadotropin (hCG), and Lactate dehydrogenase (LDH), can strongly indicate the presence of testicular cancer. However, it's important to note that these markers may not be present in all cases, so their absence does not necessarily rule out cancer.
Computed Tomography (CT) Scan
CT scans are used to check whether testicular cancer has spread to nearby or distant tissues. If there is suspicion of testicular cancer based on examination and tests, the testicle may need to be removed for a definitive diagnosis.
What Are the Treatment Methods for Testicular Cancer?
The treatment of testicular cancer involves both diagnosis and management and typically includes the surgical removal of the testicle through a procedure known as radical inguinal orchiectomy, which is performed through an incision in the groin. However, other treatment methods for testicular cancer include:
Surgical Treatment
In advanced or high-risk stages of cancer, retroperitoneal lymph node dissection (a surgical procedure to remove abdominal lymph nodes) may be recommended for some men.
Chemotherapy
Chemotherapy drugs may be required to treat cancer cells that have spread beyond the testicles. Additionally, some patients may receive chemotherapy as an adjunct treatment after surgery.
Radiation Therapy
Radiation therapy may be recommended as a treatment option for some testicular cancer patients, particularly those with seminoma-type cancer or when used in combination with chemotherapy or surgery. Additionally, radiation therapy can be used in cases where metastasis is present or surgery is not suitable.
The treatment of testicular cancer is a personalized process that depends on various factors, including the extent of cancer spread, the type of cancer, and the patient's overall health. For early-stage testicular cancer, surgery to remove the testicles is typically the primary treatment option. Surgical procedures that involve the removal of only one testicle do not lead to complications in patients. Some patients may worry about infertility or erectile dysfunction after the removal of one testicle, but this is generally not a concern. However, it's important to note that the removal of both testicles can lead to infertility.
In cases where cancer cells have spread to lymph nodes, the lymph nodes can be removed through surgery. This procedure does not typically result in erectile dysfunction. In addition to surgical methods, radiation therapy and chemotherapy may also be used, especially for seminoma-type testicular cancer and in cases where metastasis is present.
 Türkçe
Türkçe
 English
English